Over the course of the last week, I have been working on healthcare research. We finished our report on the maturation of hospital supply chains, and I have put the finishing touches on the Healthcare Supply Chain Index for this Thursday’s webinar. I also had the opportunity to speak at the GHX conference and facilitate a leadership workshop on the required changes for implantable devices. As I worked with healthcare leaders, and shared the research available on slideshare, I better understood the individuals’ pain.
Here are some of the quotes from the workshop I led yesterday that helped me to better understand the industry:
- “A process born out of chaos is chaos. The problem is us. We have to change the mental model of our organizations to move forward.” Medical Device Manufacturer
- “Does everyone realize how bad the problem is? We cannot process map ourselves out of this problem, it requires new thinking.” New Supply Chain Leader of a Regional Children’s Hospital
- “We have used Lean process systems and swim-laned ourselves to death. Today, we are efficiently swimming in the lanes without alignment on value-based outcomes.” Supply Chain Leader of a Large Hospital
- “We are a large part of the problem. We cannot drive change without taking a hard look at ourselves. It starts with redefining our processes and what we reward.” Supply Chain Leader of a Large Hospital
Healthcare is at a pivotal transition point. I firmly believe that supply chain leadership can make a difference. Over the last decade, power shifted in the healthcare value chain. Originally healthcare suppliers sold to physicians. At the dawn of the decade, the supplier had the power. In the last five years, while the physician is still important, the buying decisions transitioned from the supplier to the care provider. It is now shifting again. With the introduction of managed care, the transition of power is to the payer. It needs to shift to the patient.
No one questions the statement that managed care will dramatically affect the healthcare value chain. The change will not be incremental: It will be a step change. Hospital receivables will lengthen and supply chain roles within the hospital will become more important. The traditional focus on efficient sickness will shift to health and wellness. It requires a redesign, from inside-out to outside-in, based on value-based outcomes. The change in accountable healthcare will give more voice to the patient. Data driven discussions on patient satisfaction, readmittance rates and hospital-induced infections will be transformative.
The question in front of us is “How do we get started?” Hospitals are fragmented. They are small regional players. While processes have matured, it is hard for individual healthcare providers to get traction.
Suppliers now have a dance partner. But, the tune has changed, and they are unsure how to dance together. Hospital supply chains have matured. Seventy-five percent of hospitals have a supply chain organization. The average tenure of the supply chain professional in the hospital is six years. Hospital supply chain teams have 1/3 the tenure of the supplier’s supply chain organization. The most common reporting relationship in the organization is to the hospital’s Chief Financial Officer (CFO). The most common reporting relationship in the supplier organization is to a leader of supply (focus on logistics, distribution, materials sourcing and customer service). The focus has been on sourcing and managed costs. They lack the greater understanding of planning and value network design. While hospital supply chain organizations have made progress in the last decade, the gap has widened between the supplier sectors of pharmaceuticals and medical device manufacturers and other manufacturing industries.
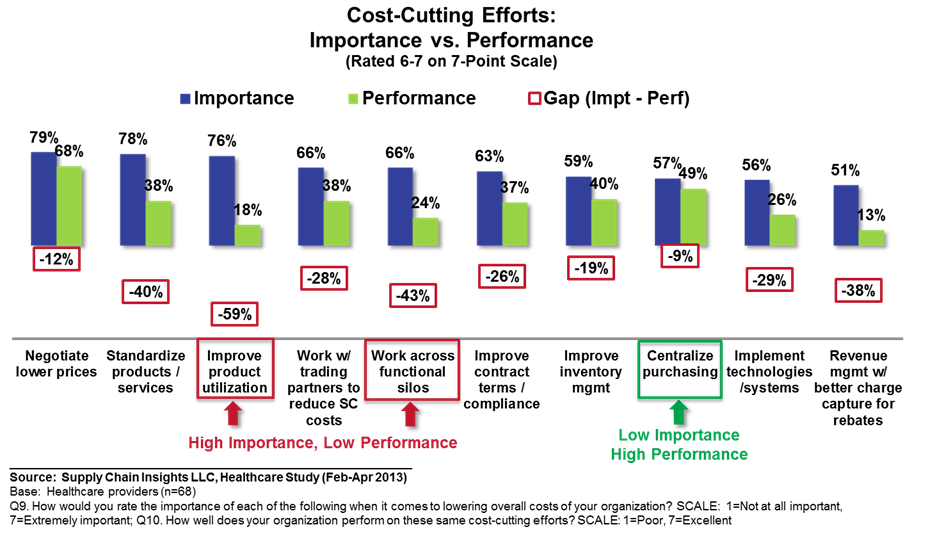
For suppliers, the focus has been on the supply chain organization as a function, not the building of end-to-end processes. Both sets of trading partners have concrete mental models that define the supply chain. For the hospital, the focus has been on materials management and negotiating of lower costs. While 72% have a value analysis team, they have not matured to assess value. These processes are still in their infancy. They are primarily focused on cost management on new purchase decisions. By and large, they struggle to gain cross-functional alignment on process redesign to improve outcomes. They lack the understanding of continuous improvement programs and struggle with alignment.

Most care providers are working to get physician and clinical alignment to focus on the right balance of standardization, product utilization, and innovation. The historic practice of incentives for direct payment to physicians drives bad behavior that is hard to control. Through employee downsizing and consignment-based sales, they have shifted costs to the suppliers. These costs now lack controls. The answers to healthcare are about much, much more than process mapping.
In contrast, suppliers are large and global players. Over the course of the last five years, they have fought the shift in power. In fighting for every sale they have become very sales-driven. They have taken on consignment-based sales without redesigning processes outside-in. (In exchange for acceptance of a consignment model, suppliers could have redesigned processes to enable better sharing of daily usage and case scheduling on a daily basis.) The mental model is one of supply. For the supplier team, they see the supply chain as a function. They struggle to define end-to-end processes. The teams fight for recognition to participate in top-to-top meetings. In the evolution of supply chain excellence over the last decade, the gap in core capabilities to drive supply chain excellence has grown between healthcare suppliers and other industries. They have lost core talent while the industry is facing a talent shortage.
There are new challenges:
- With managed care, in the United States, the hospital will bear the costs of infections from hospital stays. The standards for accountable care are evolving.
- 63% of hospital operating room costs are implantable devices. The supply chain for implantable devices is complex and immature.
- Pharmaceutical products are growing more complex. Cold chain capabilities and serialization require a redesign in product handling and supply chain execution.
- The industry has created the most complex rebate incentives of any industry value chain. The administration of bifurcated trade is a barrier to the improvement of trading partner relationships. The changes in reimbursement make this even more complex.
- Pharmaceutical companies are facing a patent cliff with a 24% decline in operating margins over the last decade.
What should Companies Do?
This cannot be about process mapping and improvement of the current state. It requires a shift in the mental model and leadership. New models are required. This is both an opportunity and a risk for existing organizations:
| Do | Don’t |
| Focus on value-based outcomes of accountable care and map the processes outside in. Question conventional models. Be open to the use of new technologies, the evolution of processes, new business models and the disintermediation of existing trading partner relationships. | Accept the definitions of processes and relationships of the industry. Limit your focus to the current definitions within the hospital or supplier organizations. The value chain is lacking supply chain leadership. Both sets of trading partners have grown up with a mental model of supply without an understanding of design and demand. |
| Balance innovation and standardization. Get clear on the difference between sales-driven and market-driven initiatives. Reward supplier companies that enable innovation. Engage in data-driven discussions and actively design and participate in pilots. | Lose sight of the patient and outcomes. Use unstructured text mining and learning systems to drive data-driven discussions of innovation. |
| Adopt standards; work on effective connectivity, and share daily data daily with trading partners. Reward companies that use the data through the design of new opportunities and price brackets. | Accept conventional practices and models. |
| Reduce the complexity with bifurcated trade. Eliminate rebates, direct payments and services. | Buckle to sales tactics and conventional relationships policies. |
| Map the entire supply chain and understand the costs, drivers and waste. Be sure to not overlook the inventory carrying costs and the impact of demand latency. Have the courage to have a different discussion in top-to-top meetings. | Generalize procurement of materials. Understand the usage and the link to accountable healthcare. |
| Work cross-functionally to gain a common understanding of the impact of accountable healthcare. Share financial and use data and engage in active continuous improvement programs around care. | Look at the purchase of materials as a buy-sell transaction. |
The good news is that trading partners want to get started. There is a compelling event to move a fragmented industry forward. The challenge is changing the mental model to move from supply-centered processes focused on transactions to more holistic supply chain thinking based on value-based outcomes.
For more on healthcare, check out our recent webinar.
If you are a healthcare supplier, we would love to hear your voice in the research that we are doing on supply chain practices. Please let us know your thoughts in our confidential survey.(If you share the data with us, we will be glad to share the data with your team.)
Please use this link: http://tinyurl.com/sci-hlt-lc
Some helpful reports include:
Supply Chain Metrics That Matter: The Cash-to-Cash Cycle
Published by Supply Chain Insights in November 2012.
Supply Chain Metrics That Matter: A Focus on the Pharmaceutical Industry
Published by Supply Chain Insights in December 2012.
Supply Chain Metrics That Matter: Driving Reliability in Margins
Published by Supply Chain Insights in January 2013.
Supply Chain Metrics That Matter: A Focus on Hospitals
Published by Supply Chain Insights in January 2013.
Supply Chain Metrics That Matter: A Focus on Medical Device Manufacturers
Published by Supply Chain Insights in February 2013.